This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Gene engineered cell therapy developed to target brain metastatic melanomas
Overall survival for patients with melanoma that has spread to the brain is only four to six months. Immunotherapies, which harness the power of the immune system to attack cancer cells, have garnered excitement in recent years for their potential to revolutionize the treatment of metastatic melanomas, but results from early clinical studies indicate that the prognosis for most patients remains poor. Now, scientists from Brigham and Women's Hospital, a founding member of the Mass General Brigham healthcare system, have integrated multiple therapeutic approaches to more effectively target melanoma in the brain. In preclinical studies, the scientists successfully activated immune responses in sophisticated mouse models that mimic human settings. Findings are published in Science Translational Medicine.
"We know that in advanced cancer patients with brain metastases, systemic drugs, given intravenously and orally, do not effectively target brain metastases," said corresponding author Khalid Shah, MS, Ph.D., director of the Center for Stem Cell and Translational Immunotherapy (CSTI) and the vice chair of research in the Department of Neurosurgery at the Brigham and faculty at Harvard Medical School and Harvard Stem Cell Institute (HSCI). "We have now developed a new immuno-therapeutic approach that is sustainable and delivered locally to the tumor. We believe that locally delivered immunotherapies represent the future of how we will be treating metastases to the brain."
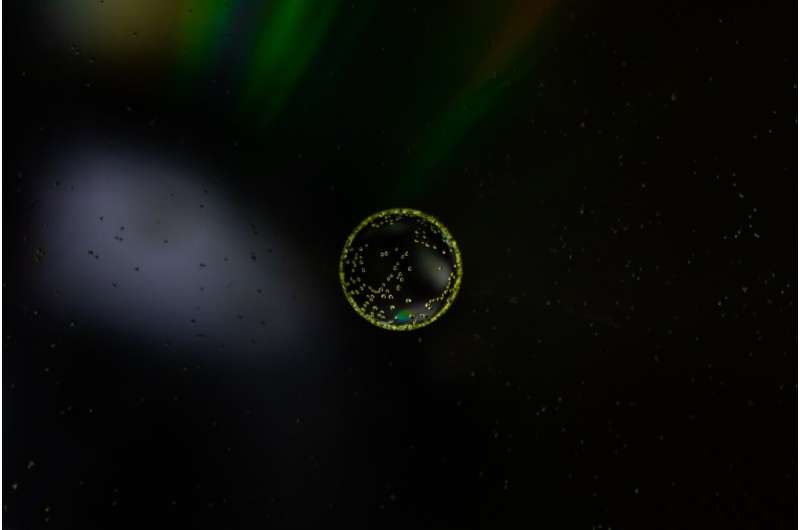
The therapy designed by the scientists uses an engineered "twin stem cell model" to maximize an attack on cancer cells that have spread to a part of the brain known as the leptomeninges. One stem cell releases a cancer-killing (oncolytic) virus, a strategy that has previously shown promise in reducing tumor growth. Using stem cells to deliver the virus amplifies the amount of virus that can be released and ensures that the virus will not be degraded by circulating antibodies before it is released on the cancer cells.
However, the oncolytic virus also destroys the very cells that release it, making it an unsustainable therapeutic option on its own. Therefore, the scientists used CRISPR/Cas9 gene editing to a create a second stem cell that cannot be targeted by the oncolytic virus, and which instead releases proteins (immunomodulators) that fortify the immune system to help fight off the cancer.
The twin stem cells can be delivered via intrathecal injection, a technique already used in the treatment of other diseases. Unlike other immunotherapies that have emerged in recent years, it does not need to be repeatedly administered. The authors emphasize that this approach can be used in other cancers with brain metastasis, such as lung and breast cancer, and are working to design similar treatments for these cancers.
Notably, the authors were able to design a preclinical mouse model that faithfully represents a human model of melanoma with leptomeningeal metastasis, which they used to test their therapy. They found that the therapy successfully activated immune responses in their models that mimic human responses, improving the likelihood that the therapy may succeed in a Phase I trial, which the authors are hoping to launch in the near future.
"A number of biological therapies that look promising often fail in Phase I or Phase II clinical trials, in part because the preclinical models do not authentically replicate clinical settings," Shah said. "We realized that if we did not fix this piece of the puzzle, we would always be playing catch-up. I don't think we have been at a point in the last 20 years where we have been as close to curing metastases in the brain as we are now."
More information: Nobuhiko Kanaya et al, Gene edited and engineered stem cell platform drives immunotherapy for brain metastatic melanomas, Science Translational Medicine (2023). DOI: 10.1126/scitranslmed.ade8732. www.science.org/doi/10.1126/scitranslmed.ade8732


















